Egg Donation
What is Egg Donation?
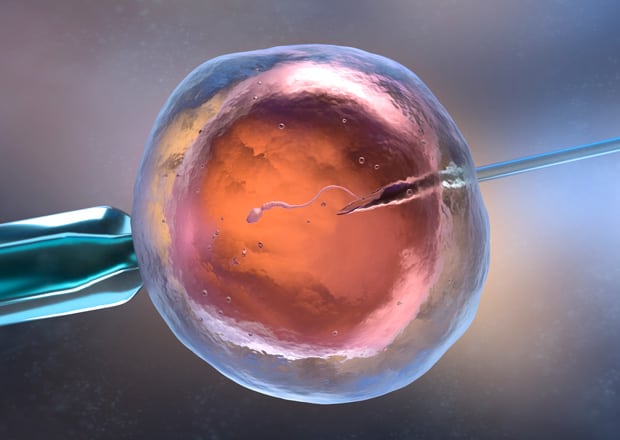
In Vitro Fertilisation with donor eggs, or Egg Donation, involves obtaining and fertilising eggs from a donor outside the body of the female who is going to receive them by means of a simple procedure.
The donor eggs will be fertilised using spermatozoids from the patient’s partner or with donor sperm from the Sperm Bank. Once fertilised, a limited number of the resulting embryos will be transferred to the recipient’s uterus where they can continue to develop naturally.
How Egg Donation works
Egg Donation makes it possible for women to make their dream of motherhood come true when they have no other options.
Egg Donation is an altruistic act, meaning the recipient cannot bring her own donor or choose who her donor will be. Likewise, the donor cannot receive any payment for her donation. For legal reasons, donor anonymity shall be guaranteed under all circumstances.
When is Egg Donation indicated and what are the phases?
Absence of ovarian function
Recurrent miscarriage
Genetic abnormalities which contraindicate the use of own eggs
Previous unsuccessful in vitro fertilisation cycles
Women of advanced age or women in menopause
Premature ovarian failure or poor response to ovarian stimulation in IVF
PHASE I: SELECTION AND ASSIGNMENT OF THE DONOR
Selection of the egg donor is a task that always corresponds to the medical team, who guarantee that the selected donor will be as compatible as possible and will resemble the recipient and her family’s physical and immune characteristics as closely as possible. All donors are between eighteen and thirty-five years of age, have the full capacity to act and are in good psychophysical health. In order to ensure their health, all donors undergo thorough medical and gynaecological exams as well as a comprehensive test for genetic markers.


PHASE II: ENDOMETRIAL PREPARATION OF THE RECIPIENT
The recipient’s uterus is prepared using hormone replacement therapy. The treatment process is monitored with ultrasound scans and hormone testing.
PHASE III: DONOR EGG RETRIEVAL AND EMBRYO CULTURE
Once there are an appropriate number of follicles which have reached the ideal size we will schedule the donor’s egg collection to retrieve the eggs.
The sperm sample, whether from the patient’s partner/spouse or from the Sperm Bank, is processed in the laboratory to select the best spermatozoids. The eggs can be inseminated with spermatozoids using Classic IVF or sperm microinjection (ICSI), which involves injecting one pre selected spermatozoid into the cytoplasm of a mature egg.
The day following egg retrieval we will be able to determine the number of fertilised eggs, or pre embryos. The embryos will remain in conventional incubators for three to five days with CO2 and temperature controls, or in a Time Lapse EmbryoScopeTM incubator. Laboratory staff will be in contact with the patient at all times to keep her informed about embryo development.

PHASE IV: EMBRYO TRANSFER AND PREGNANCY TEST
The embryo transfer consists in placing the best embryos inside the uterine cavity by entering through the vagina. It is a painless, outpatient procedure that does not require sedation or hospitalisation. It is carried out in the operating theatre and lasts about ten minutes. Following the procedure the patient will continue taking hormone treatment to favour the viability of a possible pregnancy.
In the event that the patient has additional, good quality, viable embryos, they will be cryopreserved (through a process called vitrification), allowing for a frozen embryo transfer in the future. The pregnancy test can be performed 16 days after the donor’s egg retrieval has taken place.
Clinical Results 2022
Our excellent results are the best letter of introduction to any patient. That is why we collaborate with the registry of the Spanish Fertility Society, and each year we send the results of all our assisted reproduction techniques.
IVF-ICSI | Donor Eggs
CUMULATIVE PREGNANCY RATE PER CYCLE (frozen embryo transfer included)IVF-ICSI | Donor Eggs
CUMULATIVE PREGNANCY RATE PER ATTEMPT (last 3 years)More info
Complete the form or call us at (+34) 952 122 565.


